Author: Dott. Riccardo Rosa
Anamnesis
38 year old boy. Communication and marketing expert. Computer “dependent”. He hasn’t been exercising since December. With the lockdown his amount of work on the computer had increased by 3 hours a day.
Three weeks before the visit, after a sudden movement at the end of the shower, the patient reported that he felt a deep pain between the right scapula and the spine. No “strange jolt-like” sensation (experienced in the past) along the corresponding arm, but he felt a sensation of “muscle soreness” in the area of the right biceps and pectoral muscles. He also reported severe functional limitation (“completely blocked and sore”). He took anti-inflammatory drugs for a few days but with no obvious benefit.
In the days following the acute episode, the mobility was improving overall but a form of unilateral right headache, diffuse, vague (heaviness) starting from the middle cervical and right scapular area, and an occasional sensation of “Instability”, “staggering” (lying on the sofa with head back). As this was a new relapse (the third block in a few months) and the situation was slow to resolve, the home remedies and medications did not seem to improve the condition, he decided to visit my office.
Movement in general helped him, and symptoms and mobility seemed to worsen towards the afternoon and evening. At night he could feel the sensation of hands falling asleep and in the morning the awakening was stiff and painful. The patient himself reported a correlation between the time spent sitting working on the PC, certain postures and symptoms.
The intensity of the symptoms was not the main problem for the patient and the mobility was already progressing. His coping ability, that is the way he controlled and dealt with his condition was “positive” and he declared himself very willing to receive active indications (exercise) just to get better and not “relapse”. The main reason for his visit was precisely: “I would like to understand how to avoid making such a foolish comeback”.
Test with baiobit:
After the general medical history and the exclusion of serious problems (red flags) in progress that could have required a specialist visit with a doctor, the functional evaluation of the active movements was performed.
Cervical ROM with baiobit
Each movement was repeated 3 times using verbal commands with external focus (eg: “go and look at the window curtains on the right”).
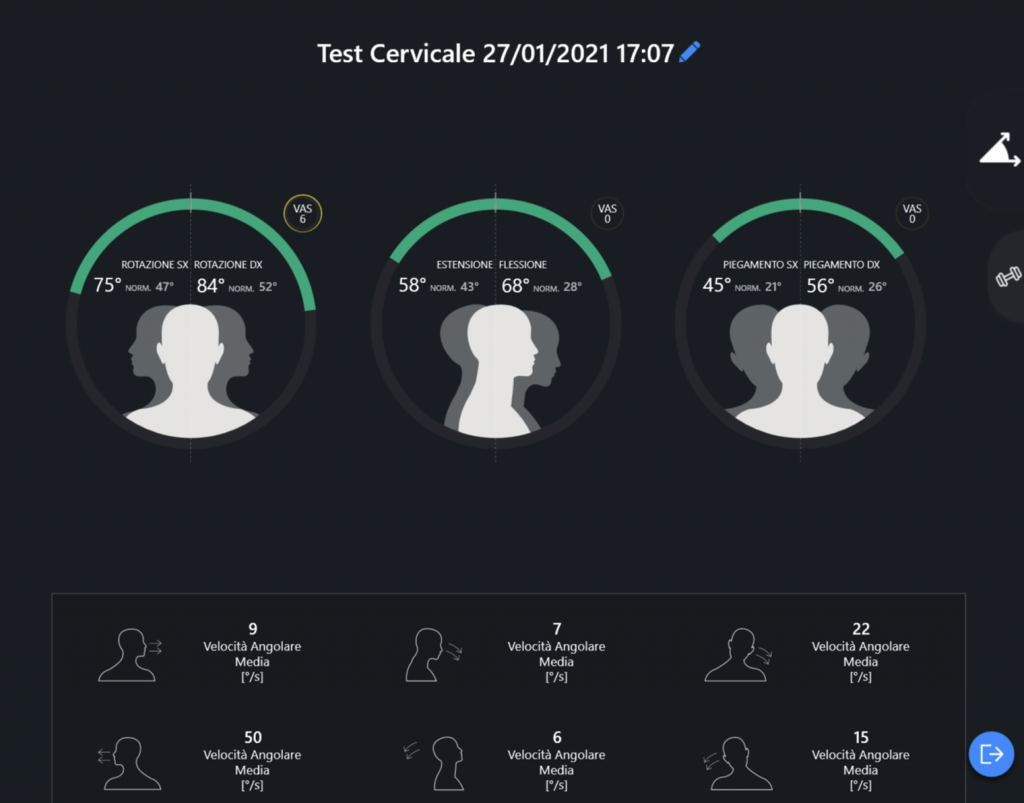
Overall, mobility did not appear to be functionally significantly impaired, quite the contrary. (ROM measured in the norm).
In particular, a good range on the various planes was highlighted with some differences between the execution speeds, indicative of adaptive or otherwise different motor control strategies.
The provocation of the patient’s familiar symptoms was possible in the right rotation (local pain and shoulder blade), extension (dizziness) and retraction (combined movement not measured with baiobit) patterns.
Clinical physical examination: Excluding various differentiation tests, evaluation of regional and segmental passive movements was performed, and provocative soft tissue palpation tests which confirmed the presence of numerous hypersensitive and provocative myofascial areas associated with dysfunctions and hypersensitivity of corresponding segments articular at the level of the upper cervical (segment C2-C3), medium (C3-C4), at the cervico-thoracic level (C7-T1).
Treatment
Treatment of the first and second sessions included: cervical LVLA mobilization techniques, cervical and thoracic HVLA manipulation techniques manual neuro-muscular techniques to restore joint mobility and district and regional dermo-neuro-myofascial extensibility. Manual therapy was associated with 3 exercises performed with the assistance and supervision of the therapist: a mobility exercise, a neuro-motor control exercise in cervical rotation and an exercise in cranio-cervical, cervico-thoracic retraction + step extension.
Results
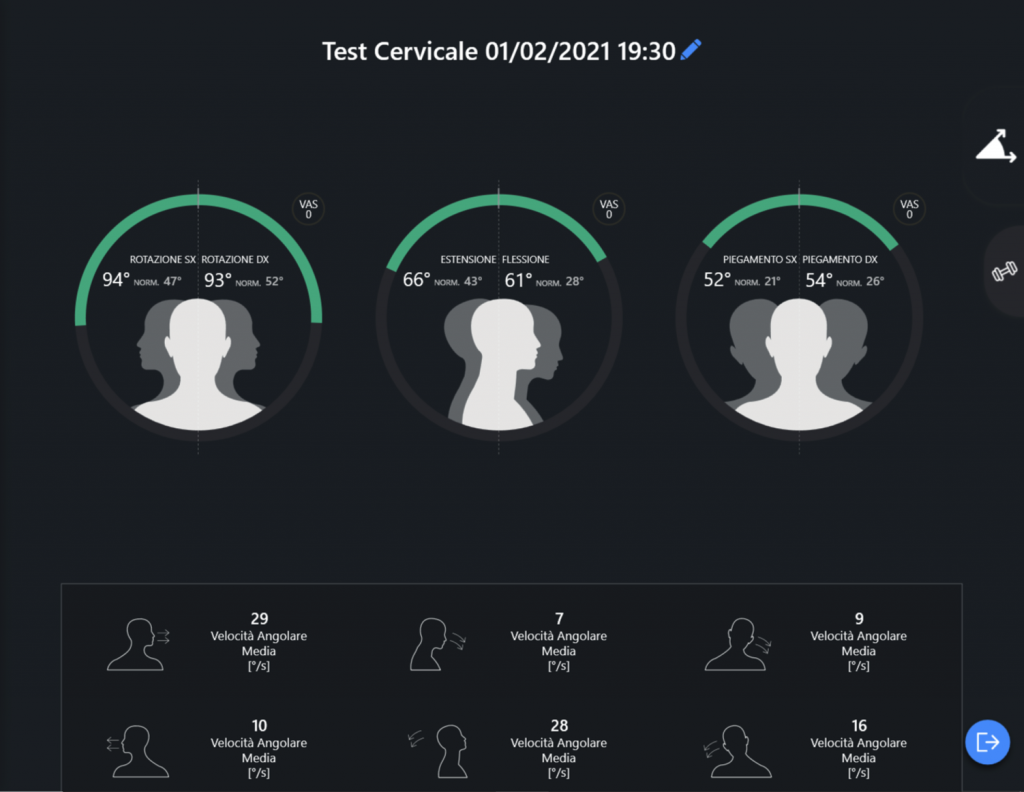
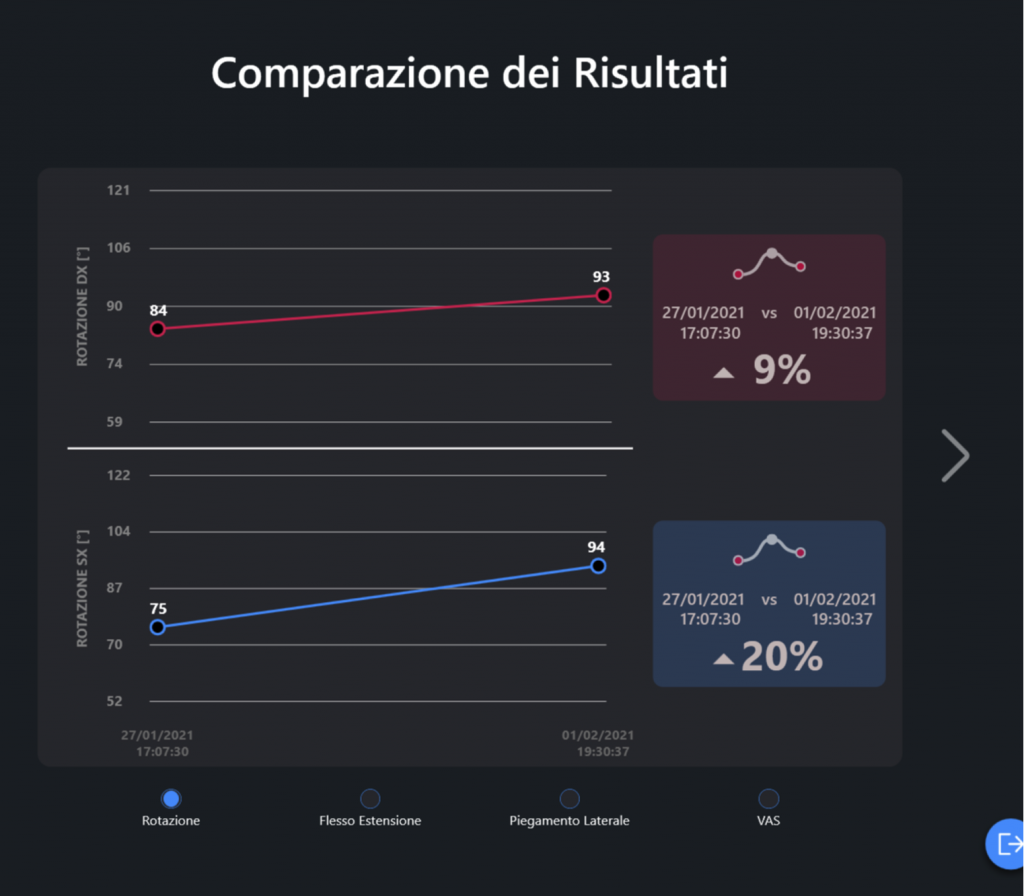
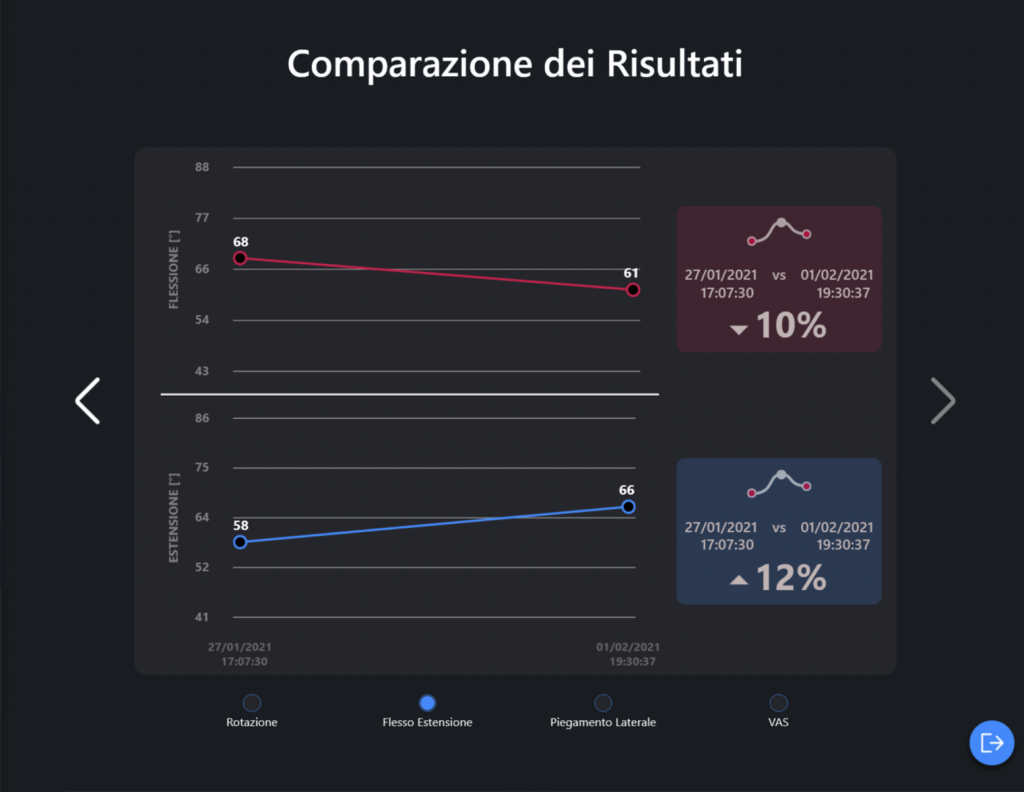
The data from the comparison of the Movement Test with baiobit demonstrate in 2 sessions the elimination of painful symptoms and “dizziness”, and a further improvement as well as a more homogenous “distribution” of the ROM, especially in the sagittal plane between extension and flexion, indicative of a reorganization of the neuro-muscular coordination strategies. The increased speed of execution in the extension movement indicates an overcoming of the fear of executing it confirmed by the patient himself.
It should be noted that the pre and post treatment visualization of the objective data collected with baiobit by the patient amplified the perceived therapeutic effects (objective feedback effect) and the perception of the difference as well as the value of the therapies carried out and the path taken (to the advantage and benefit of the professional’s reputation). The patient was in fact used to “different cycles of physiotherapy” but thanks to the results obtained and the objective evidence of the improvements achieved, he particularly appreciated the proposed strategy and the rehabilitation therapy administered.
Initial cervical evaluation with the baiobit system
Cervical evaluation at the end of the rehabilitation process with the baiobit system
Comparison of the cervical range in initial rotation and at the end of the rehabilitation process
Comparison of the cervical range in flexion, initial extension and at the end of the rehabilitation process
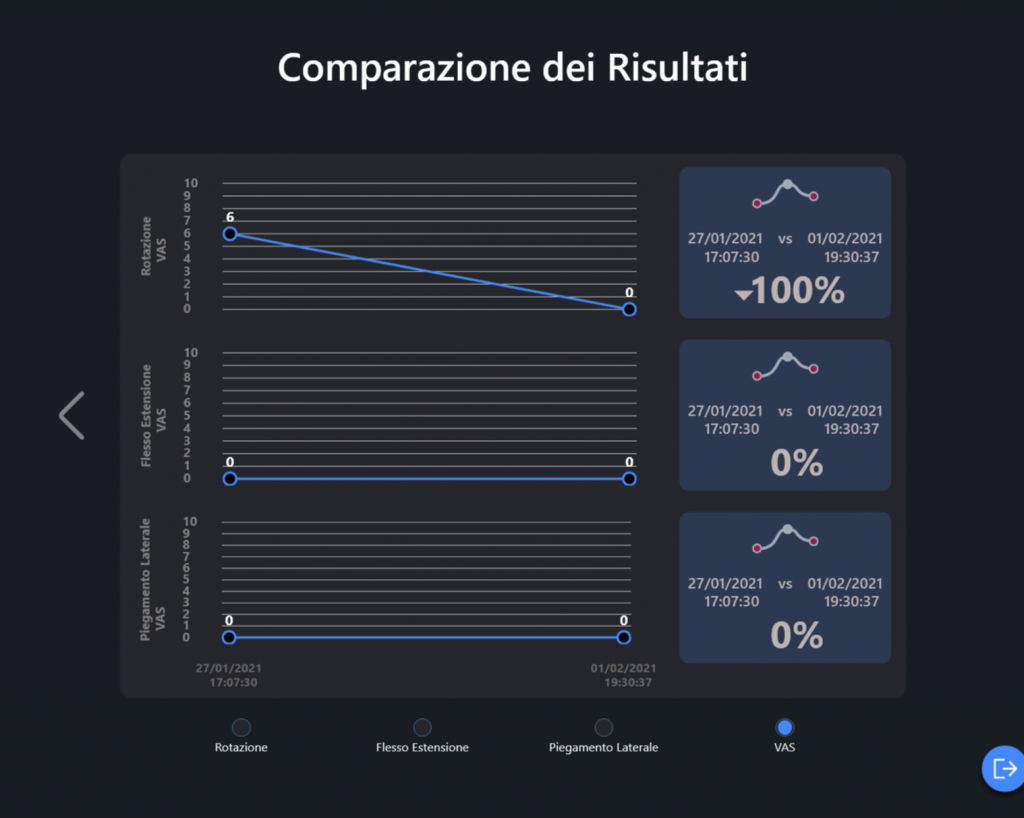
Comparison of pain measured with VAS scale in the three directions of movement in the initial phase of therapy and at the end of the rehabilitation cycle